Article written by: Doris Murimi
I find it shocking that menstrual hygiene management discourse hardly ever includes menstrual disorders knowledge. Yet, in my view, the connection is clearly so blatant. I keep asking myself how do the MHM people miss it? Then I remember that there is the common saying that only the wearer of a shoe knows where it pinches. Implying that those that have experienced something, are more likely to be aware of it. So having suffered from menstrual disorders I will explain the connection between menstrual disorders and menstrual hygiene. It is my hope that this will result in more inclusion of menstrual disorders education/knowledge within menstrual hygiene management.
Briefly, the four basic classifications of menstrual disorders are:
One, is Abnormal Uterine Bleeding (AUB) and according to ACOGis divided into two categories. The first one, heavy menstrual bleeding (which replaced the term menorrhagia) results in menses which last over 7 days in duration or are over 80ml in terms of flow measurement. The other one which replaces the term metrorrhagia is intermenstrual bleeding which is considered to be any bleeding that occurs outside the menstrual cycle. Some causes of AUB are fibroids, adenomyosis and uterine polyps.
Two, Premenstrual Syndrome (PMS) refers to physical and psychological symptoms that are severe and disruptive and related to the menstrual cycle. About 30 to 40% of women are affected by PMS. A more severe form of PMS isknown as Premenstrual Dysphoric Disorder (PMDD) which requires medical attention. It is described in this way. If PMS is like a bad tension headache then PMDD would be considered a migraine. It is said to affect 4 to 8% of women.
Three, Dysmenorrhea which refers to painful menstruation (Both Primary and Secondary). Primary dysmenorrhea is the name for common menstrual cramps and is linked to the ovulation process. Secondary dysmenorrhea is caused by an underlying gynecologic disorder such as endometriosis, adenomyosis, fibroids and Pelvic Inflammatory Disease.
The fourth one is Amenorrhea (Both Primary and Secondary). In the case of primary amenorrhea this is generally related to either the absence of menses or late commencement of menses such as at 16 years of age and over. In the case of secondary amenorrhea, menses are normal and regular for a duration but become increasingly abnormal and irregular e.g. they suddenly stop for three months or longer.
So with this background, when we look at menstrual hygiene management, we should consider factors such as heavy bleeding as a definite correlating factor of menstrual hygiene. In a research study on Knowledge and menstrual hygiene practice among adolescent school girls in southern Ethiopia: a cross-sectional study (https://doi.org/10.1186/s12889-019-7973-9), the findings showed that the odds of having poor menstrual hygiene practice among adolescent school girls with longer duration of menstrual flow were 2.51 times higher as compared to girls with shorter duration of menstrual flow. The possible explanation for this association might be due to the fact that girls with longer duration of menstrual flow may have economic constraints to buy commercially made absorbents for longer time.
In addition, the research findings showed that longer duration of menstrual flow may affect the psychological and emotional states of girls which may further diminish their motivation and commitment to perform safe hygienic practices. I would also imagine that girls with dysmenorrhea, PMS or PMDD may also be psychologically affected in this similar manner.In fact the study showed that large proportions, 615 (77.7%) of adolescent school girls in Gedeo zone mentioned that they had experienced dysmenorrhea (severe pain during menstruation) at least once within the last three consecutive menstrual cycles.

Similarly, the same study found that the odds of poor menstrual hygiene practice amongst adolescent school girls who were aged less than 15 years was increased by 1.71 times as compared to girls whose age was equal or greater than 15 years. Accordingly, this is possibly explained by the fact that girls ofolder ages can have better opportunity to share more information, gain adequate knowledge regarding menstrual hygiene, and prepare themselves to demonstrate safe hygienic practice during their menstruation period as compared to younger girls.
The main focus of this study was whether knowledge towards menstruation has significant associations with menstrual hygienic practices of girls. The findings from the study actually confirmed this by showing that girls with poor knowledge regarding menstrual flow were 1.48 times more likely to practice their menstrual hygiene incorrectly. Accordingly, this is possibly due to the effects of cultural beliefs and social taboo regarding menstruation and its hygienic practices attributed by the community they live. In India for example, the avoidance of pollution of water sources on religious basis is a possible reason why menstruating women are not allowed to take a bath especially for the first few days of their menstrual period. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4408698/).
In conclusion, the study which covered a total of 791 girls, found that majority of the adolescent school girls had poor knowledge regarding menstruation and their hygienic practices were incorrect. Lower age, longer duration of menses flow and poor knowledge towards menstruation were significant correlates of poor hygienic practice. This study demonstrates a need for the design of acceptable awareness creation and advocacy programs for adolescent school girls and the public to improve the knowledge and safe hygienic practice of menstruation flow.
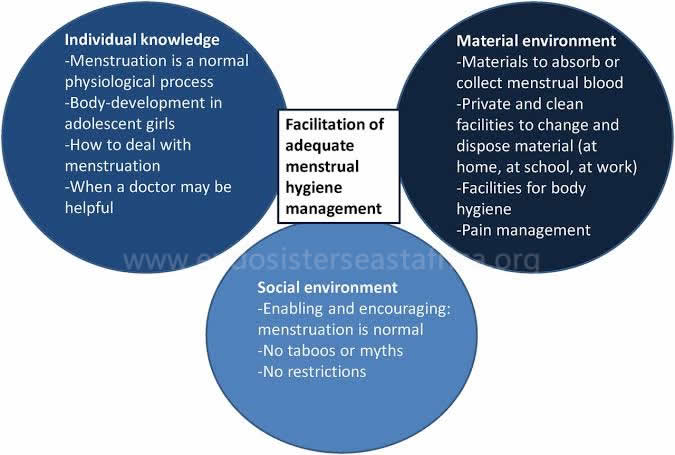
In my view, a key aspect of that essential knowledge that the researchers refer to is found in menstrual disorders education. Unfortunately, from what I have seen, majority of the menstrual hygiene management policies operate from the premise that all girls experience normal menstruation. Why? Because they tend to prescribe a one size fits all approach to menstrual hygiene. I would argue that in order to design more effective menstrual hygiene interventions, it is important to include menstrual disorders education as essential knowledge.Why do I say this? The menstrual hygiene practice for a girl with normal menstruation versus one with heavy menstruation should be addressed differently. It may be necessary for the one with heavy menstruation to bath twice a day, increase the frequency of changing sanitary pads, use more appropriate materials to minimize leakage, budget more for sanitary protection, increase the number of school uniforms, have a mechanism to deal with odours emitted, etc.
For the girls with dysmenorrhea, prescribing pain medication as well as providing them with appropriate medication for underlying conditions such as endometriosis could very well improve their motivation to observe better menstrual hygiene. This is because with treatment they are in a better frame of mind to improve on their menstrual hygiene. The pain from some of these conditions can be so excruciating that it completely makes it impossible for a girl to attend to daily things such as observing good hygiene. The same would apply for girls who suffer from PMS or PMDD. If one has depression as a result of PMS then obviously personal hygiene is usually one of the first things that is compromised. To be honest, the likelihood of a girl having HMB, dysmenorrhea and PMS all at the same time is also very likely.Let us also not forget the girls experiencing amenorrhea who may think that menstrual hygiene does not really apply to them especially those with primary amenorrhea as they do not experience menstruation at all or regularly. Since they lack the essential knowledge informing them that puberty changes still require improved hygiene.

So when we generalise in our interventions as a society, we make it difficult for girls to come forward. When we do not provide menstrual disorders as essential knowledge it creates a veil of shame around abnormal menstruation and girls do not know how to bring up the issue. So in my view, the solution lies in ensuring that essential knowledge comprising of menstrual disorders education is taught in schools. This will empower girls with menstrual disorders to come forward and seek medical attention sooner with no shame. It is our duty to create an enabling environment for girls to discuss these issues openly and ensure that they are provided with the right knowledge and guidance. Most importantly, it supports the designing of effective menstrual hygiene management interventions. Is this not the ultimate goal?



1 Comment
Tabitha · December 9, 2020 at 2:11 pm
Thank you for sharing. This is important information.
I agree with you, menstrual disorders education should be taught in schools.
Comments are closed.